There is just not enough Wegovy.
The current manufacturing shortage will eventually end, and those who have health insurance that covers Wegovy, plus the even luckier ones who can afford to pay out of pocket, will once again get their medication.
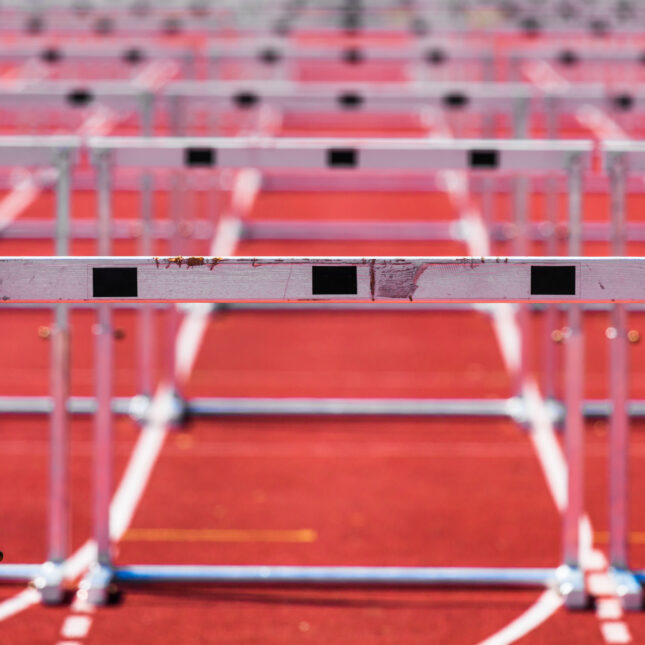
But even if Novo Nordisk were to manufacture an enormous surplus of Wegovy, millions more will never get it. Whether due to short-sightedness or seeing obesity as a choice rather than a disease, many insurance companies outright deny coverage of medications for weight loss. As an endocrinologist at an academic medical center who specializes in treating metabolic diseases, including obesity and type 2 diabetes, I try to give all my patients the best possible care against these obstacles. But medical weight management has become an endurance sport for my patients and me.
Glucagon like peptide 1 (GLP-1) receptor agonists, including the household names Wegovy and Ozempic as well as several others in this medication class (Saxenda, Victoza, Trulicity), can be very effective for weight loss and for lowering blood sugar. Despite all the hype, let’s not forget that GLP-1 receptor agonists are medications, not miracles. They have very common and unpleasant side effects, and not everyone loses a lot of weight when they take them. Still, they are undeniably game-changers in the relatively barren landscape of medications to treat obesity.
Obesity is a complex neurometabolic disease that is the consequence of much more than bad math (calories in exceed calories out). People do not choose to sit and eat their way to very high body weights. There are many other factors — genetics, epigenetics, the gut microbiome, weight-promoting medications — in the body weight equation that are overlooked. Obesity is vulnerable to judgment because you can see it.
So, physicians like me face a disease that bears the burden of bias, topped with hurdles or brick walls that drastically limit access to medications that can be very effective for weight loss. Medicare doesn’t care; it does not cover medications for weight loss, period. Wellsense, a nonprofit insurance company, makes no sense: They also don’t cover medications for weight loss. Tricare, the military health care plan, lives up to its name insofar as you have to try very hard to get the care you want: People with obesity are required to try and fail every other available medication for weight loss (many with cardiovascular side effects) before they will even consider covering GLP-1 receptor agonists.
Every day, I have a tempting opportunity to play Robin Hood and expand access to Wegovy. Wegovy and Ozempic are actually the same molecule, called semaglutide. Wegovy is approved by the FDA specifically for the treatment of obesity, and Ozempic is approved specifically for the treatment of type 2 diabetes. Novo Nordisk has issued several statements reminding medical professionals that Wegovy and Ozempic should not be used interchangeably. The tempting Robin Hood opportunity is a loophole whereby Medicare typically covers Ozempic for people who do not have type 2 diabetes. This loophole could be a release valve for my frustration over our short-sighted medical system that misunderstands obesity as a disease. As it turns out, though, it’s really robbing Peter to pay Paul, because it’s created secondary shortages of Ozempic and other GLP-1 receptor agonists approved specifically for type 2 diabetes. My own patients with type 2 diabetes are now having a hard time getting the drug that has brought them significant reductions in blood sugar levels.
Some days I want to break the rules for every patient, and other days I want to draw a line in the sand. It would be easier if I adopted an objective approach to prescribing, but I’m not even sure what that would look like. Would I prescribe Ozempic for everyone with BMI over 30? Or for everyone with Medicare? Or would I save it for patients with type 2 diabetes?
Instead, by trying to be thoughtful and offer personalized care, I feel like I am literally weighing one patient against another.
Here are real decisions I have had to make: Do I prescribe Ozempic for a patient with normal blood sugar who was told he has to lose 50 pounds before he can get a much-needed knee replacement? What about someone with breast cancer, and no diabetes, who needs to lose pounds before she can have breast reconstruction? (By the way, medications to treat breast cancer cause weight gain.) Or a patient who is more than 100 pounds overweight and has pre-diabetes, high blood pressure, and high cholesterol? How about a patient who is 35 pounds overweight, without any other metabolic diseases, but so severely depressed by his weight that he has become socially isolated and does not leave home? And the final gut punch: a 64-year-old patient with a BMI of 45 who was doing really well with Wegovy, tolerating it without severe side effects and has lost about 30 pounds, only to turn 65 and learn that Medicare doesn’t cover medications for weight loss. Who “deserves” Ozempic more? These are not decisions I want to make.
There are several new medications in clinical trials for the treatment of obesity, with exciting results so far. These new meds on the block are sure to be very expensive, and if the present, unfair landscape continues, public and many private insurance companies won’t cover them and access will be quite limited. (Medications for weight loss are notably absent from the Biden administration’s list of high-priced drugs that will be subject to price negotiations for Medicare.) More medications in the obesity management toolbox will provide more treatment options to some patients. The Wegovy supply shortage will end at some point. But for now, with limited supply, inequitable insurance coverage, and the complicated option of prescribing Ozempic off label, the wait is problematic.
But for now, with limited supply, inequitable insurance coverage, and the complication option of prescribing Ozempic off-label, patients and doctors are in a marathon that nobody signed up for. I hope my patients understand that I am navigating the course with everyone’s best interests in mind.
Jody Dushay, M.D., MMSc, is an endocrinologist at the Beth Israel Deaconess Medical Center and assistant professor of medicine at Harvard Medical School. She is also the founder and director of Wellpowered, a comprehensive wellness and weight management program.










Exciting news! STAT has moved its comment section to our subscriber-only app, STAT+ Connect. Subscribe to STAT+ today to join the conversation or join us on Twitter, Facebook, LinkedIn, and Threads. Let's stay connected!
To submit a correction request, please visit our Contact Us page.